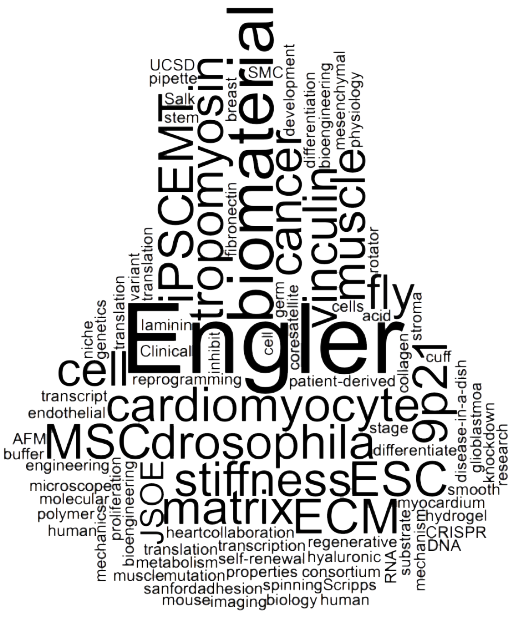
What is Mechanobiology?
Mechanobiology is the application or analysis of the role of mechanical forces in eliciting a molecular response, leading to a change in form and/or function that can be quantified. Conversely, the well-established field of Biomechanics applies forces to cells to study the mechanics of those living organisms and their components (biomolecules, cells, tissues, etc.). The Engler lab studies the mechanobiology of stem cells, progenitor cells, and their progeny as well as cancer cells using methods borrowed from tissue engineering, biomaterials, cell and molecular biology, and genetics. The field can trace its seminal roots to some of the work from the Engler lab, including some of our classic papers identifying how biomaterial stiffness influences mesenchymal stem cell differentiation and review papers defining mechanobiology.
For more information on our general efforts in Mechanobiology:
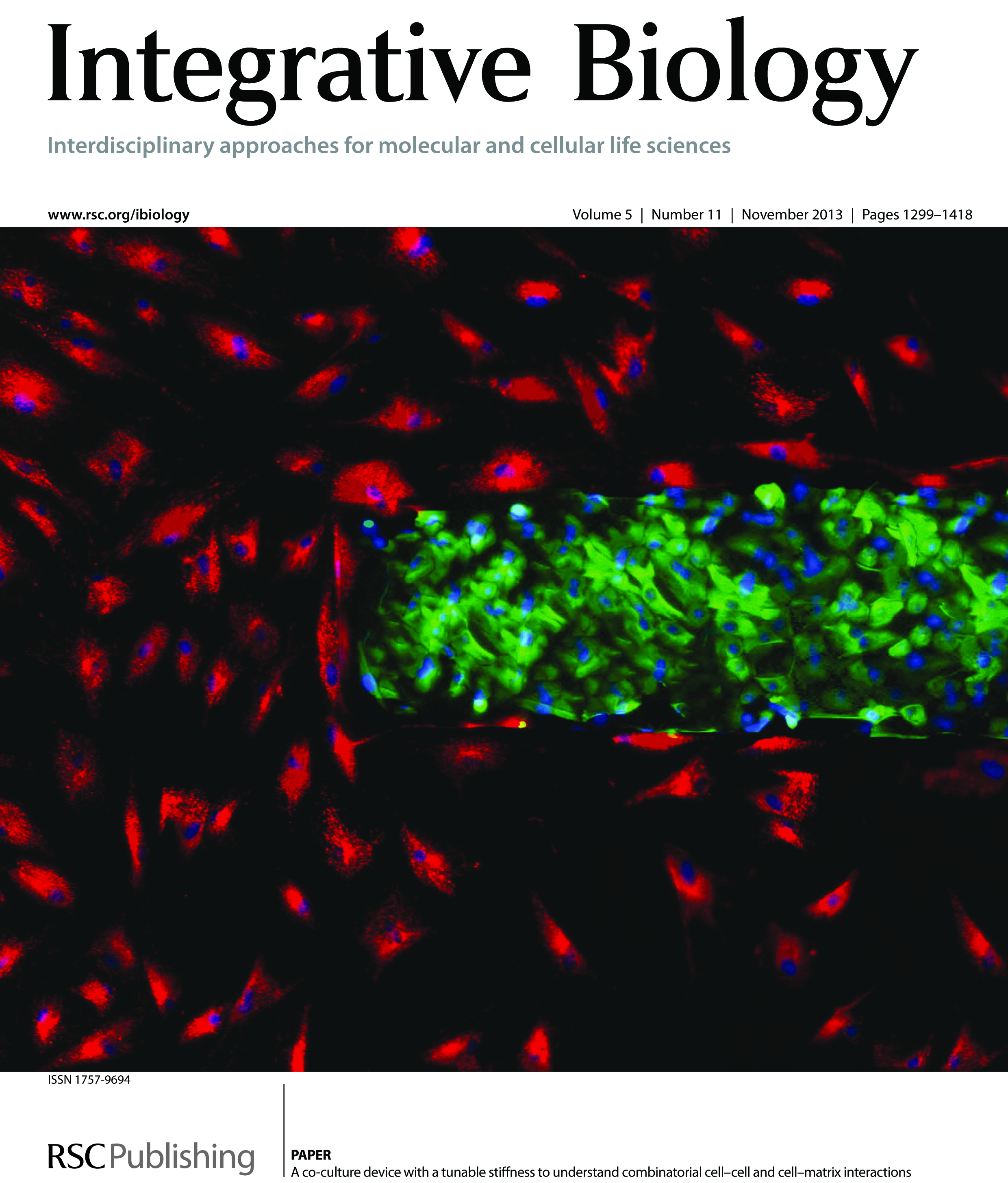
The genetic underpinnings of cardiovascular and musculoskeletal diseases
A decade ago, cells were thought to primarily respond to the growth factors and other cells that make up their environment. The Engler lab, and the broader field of mechanobiology, has shown that many cells are also sensitive to physical cues from the surrounding extracellular matrix (ECM), the fibrous scaffold to which cells adhere. We set out to determine the breadth and depth of their sensitivity to ECM properties to further this understand how physical cues guide stem cells by focusing on 1) engineering niche that are more biomimetic to better understand the extent to which ECM properties regulate stem cell fate and 2) understanding the molecular signaling involved in relaying physical ECM cues to biochemical cues for the cell.
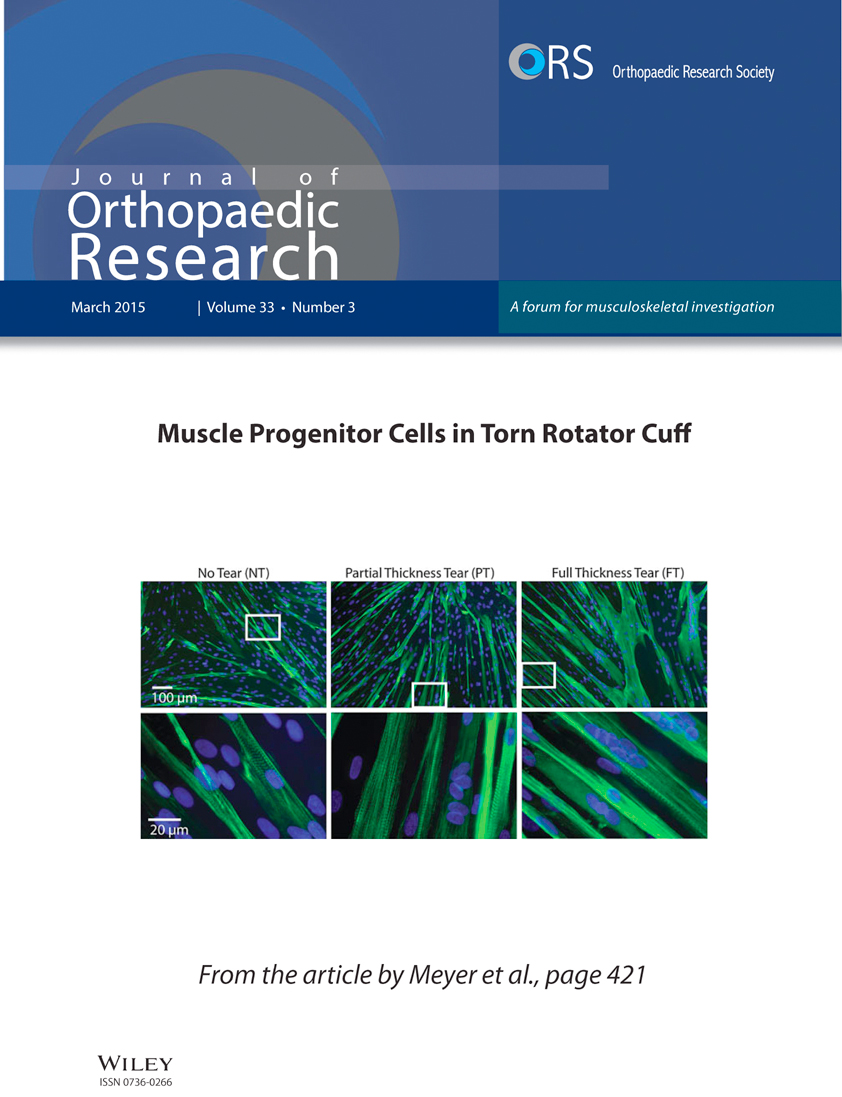
Biomaterials typically lack spatiotemporal dynamics, which normal matrix has and which may regulate appropriate tissue development. Using Michael-type addition-, free radical-, and photoactivated-based crosslinking, we have engineered polyacrylamide-, hyaluronic acid-, diblock copolymer-, and collagen-based materials to display spatiotemporal changes in stiffness. These materials enabled us to prove that developmentally or disease-specific presentation of ECM stiffness, e.g. stiffening over time or stiffness gradients, can better direct cell fate or induce the phenotypes we expect to observe from disease. Such studies improve phenotypes observed from disease-in-a-dish models of induced pluripotent stem cells (iPSCs). Working with UC San Diego and other area cardiologists, we have used our engineered materials (e.g. heart attack-in-a-dish) to observe new phenotypes in iPSCs. Some of our past efforts in skeletal muscle are highlighted in Dr. Engler's presentation at the 2013 "Stem Cell Meeting on the Mesa.”
Heart function and aging
Understand how aging affects heart function is very time consuming in mice and rats, which require years to become geriatric. Using model organisms with short lifespans, well characterized genetics, and similar cell biology to humans, we can alter our signaling pathways of interest and determine how they function in a matter of weeks. Given our expertise in cell mechanics, we have created several novel tools to understand how the heart of Drosophila melanogaster changes its function when aging from juvenile to geriatric. Despite being a rapidly aging, genetically tractable model organism with a cardiac proteome that is 82% conserved with mammals, the Drosophila heart is a soft, multilayered tube unlike humans. To be able to measure the stiffness of the tube, we developed the first linear transformation method to analyze individual layer elasticity within a soft, multilayered material by atomic force microscopy and applied it to the fly heart tube. We have also helped develop active mechanical measurements of fly physiology to assess contractile function. Using microarrays and these analysis methods, we are identifying several molecular mechanisms of age-associated remodeling at cell junctions and determining their function in flies and higher mammals to assess the conservation of those mechanisms. Flies also lend themselves well to longevity studies, which we have recently partnered with a local charter high school, High Tech High, to conduct. For more information about the project and our outreach efforts, please click below to find out more.
Understanding the onset and spread of Cancer
40% of women that have had breast cancer will relapse, due in large part to our inability to identify and control metastasizing cells; 5-year relapse rates are similar in non-small-cell lung, prostate, and other solid tumors. Recent efforts to identify molecular prognostic markers that denote metastasizing cells remain unresolved.
Metastases result from primary tumors shedding a small subpopulation of stem-like cells that can migrate through adjacent stroma and disseminate throughout the body unlike those cells remaining in the primary tumor. Progress towards identifying molecular prognostic markers of these stem-like cells that could assess metastatic risk has been limited; very recently however, evidence from our group and numerous others has suggested that a tumor’s physical state may act as an alternative prognostic marker. We have observed that one such physical marker–adhesion strength–varies in metastatic epithelial cell lines from mammary, prostate, and lung tumors due to differences in focal adhesion assembly in stromal-like conditions, e.g. low Mg+2 and Ca+2. Thus strongly adherent sub-populations are slower and less processive than their unselected counterparts. We are microfabricating new adhesion-based assays to isolate the most metastatic sub-population and develop tools to predict metastatic potential of human tumors.
At the onset of metastatic behavior, we and others have noted that the tissue stiffens in and around a tumor, making it clear that physical properties of a tissue change as tumors develop. While the genetic and biochemical events initiating cell transformation have been studied for decades, we are studying how, why, and to what extent physical environmental parameters, e.g. stiffness, drive tumor formation. Since these niche are dynamic, we use a model methacrylated hyaluronic acid (MeHA) hydrogel system that stiffens “on-demand” to mimic tumor dynamics and understand stiffness-induced epithelial-to-mesenchymal (EMT) transition.